Category: “CMS”
- CMS: Medicare ACOs continue to succeed in improving care, lowering cost growth
- Only 10% of Medicaid Enrollees’ ED Use Is Unnecessary
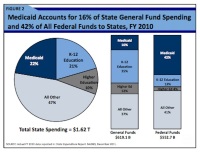
Here is government thinking for you: they start the article with ONLY. Only 10% of ED visits under Medicaid are unnecessary. As ED visits account for 4% of the Medicaid's total spend the wasted money is in the BILLIONS, that's billions, with a b. In 2012 the spend according to the Kaiser Family Foundation on Medicaid was $415,154,234,831. Four percent of that is over $16 Billion dollars, ONLY 10% of which is wasted. As they say in Washington, a billion here and a billion there and soon you're talking about real money.
- Hospitals have a target on their backs: CMS exorbitant payment to “bounty hunters
In their attempt to claw back money for Medicare and Medicad, CMS pays private auditors as part of the RAC program (recovery auditing program). Auditors get from 9% to 13% of the money they accuse hospitals of miss-billing for. Unfortunately they have a dismal record because a large percentage of claw back funds get returned to hospitals. So the question is with such a large financial incentive are the auditors making up these false charges against hospitals? AHA answers that in this whitepaper to CMS.
- Another financial roundhouse blow to Critical Access and Community Hospitals
CMS is considering reducing reimbursement once again for services that hospitals provide impacting rural and the community space the most. "Hospitals should view this move toward site-neutral reimbursement as a harbinger for the future." Pretty cavalier about taking money away from already struggling hospitals in MSR's opinion.
- ICD-10 implementation still a confusing mess even with CMS’ decision to delay implementation
- CMS spares Medicare Advantage from the Axe, at least for now
- CMS reveals Medicare physician pay data
The American Medical Association fought a 35-year battle against the release of this data. Guess they don’t believe in transparency either. Routine office visits accounted for the single largest share of Medicare physician billings in 2012 even though they amounted to just one-seventh of the $77 billion paid by the government for physician services through the nation's senior citizen healthcare program.
- Acute Care Hospital Inpatient Prospective Payment System
- Reform Update: CMS won’t limit flexibility of Oregon CCOs, state says
- ACO directory: 272 ACOs in America
- CMS claw-backs threaten to bankrupt hospitals
"Essentially it wipes out any profit we would have next year, so that's kind of why we're struggling with it," said Jackson Health System chief financial officer Mark Knight, noting the state's largest public hospital had operated in the red for years before turning things around. Jackson stands to lose $47 million in Medicaid funding with this one issue. Tampa General would be out $13.3 million.
- CMS says don’t use power strips in patient areas – ECRI says more study is needed
- Another form of rationing from CMS with 20,000 lives at stake
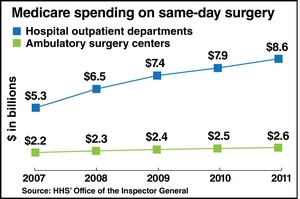
- Healthcare providers face another revenue hit as Medicare proposes to cut same-day surgery reimbursment
- President’s 2015 budget proposal: Political, not practical
"The president's budget directly counteracts the administration's efforts to reduce healthcare costs and encourage advanced manufacturing in communities across our country by instituting a burdensome prior authorization system," said MITA Executive Director Gail Rodriguez. "Inserting a bureaucratic middleman between physicians and patients will limit seniors' access to diagnostic services, while resulting in wasteful healthcare spending and fewer investments in research and development."
- Hospitals hope for relief from two-midnight purgatory
Medicare has a 2 night stay rule for patients in a hospital in order for the provider to get a higher level of reimbursement. This rule has dramatically reduced hospital admission and bed days. However it is hated by hospitals and one of the most contentious rules implemented to drive down Federal costs of healthcare. Known as the "two-midnight rule" hospitals may get regulatory relief although they want repeal.
- US Senate Report: Improving Audits – How We Can Strengthen the Medicare
- Diagnostic Imaging escapes the knife – CMS slashes at reimbursment for Radiology Oncology instead
- More Than 750 Hospitals Face Medicare Crackdown On Patient Injuries
- The AHA says the financial risks of ACO participation outweigh the rewards
- Radiology ranks No. 7 of Medicare highest-paid specialties
The information also revealed which diagnostic radiology providers earned the most Medicare dollars in 2012:
- Dr. Angelo Makris, Alexandria, VA -- $5.6 million
- Dr. Paul Svigals, Cherry Hill, NJ -- $5.1 million
- Dr. Stephen Liu, Modesto, CA -- $4.6 million
- Dr. Thanh Van, Houston -- $3.6 million
- Dr. Anthony Becker, Fresno, CA -- $3.5 million
- Dr. Robert Ivker, West Orange, NJ -- $3.5 million
- Dr. William Kelly, Palm Desert, CA -- $3 million
- Dr. John Rigney, Chappaqua, NY -- $3 million
- Dr. Patrick Browning, Sacramento, CA -- $2.9 million
- Dr. Richard Gray, Washington, DC -- $2.8 million
- Dr. Melvin Rosenblatt, Fairfield, CT -- $2.8 million
- If you sell Durable Medical Equipment you’d better read this before CMS reaches into your wallet…